World Osteoporosis Day
0 0 votes Article Rating
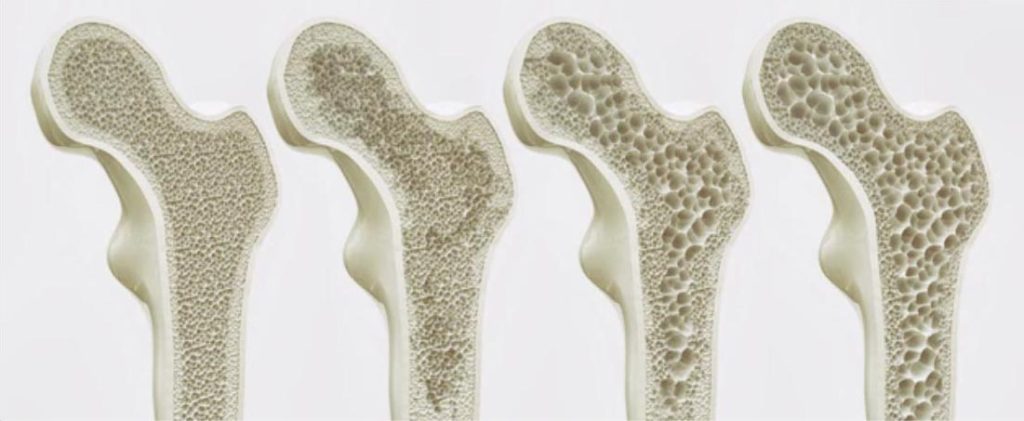
Osteoporosis is a condition that weakens the bones and increases the risk of low traumatic fracture. The gold standard for diagnosing osteoporosis is the DXA scan, which measures Bone Mineral Density and provides a classification system to identify osteoporosis or osteopenia. Common body sites that are measured include the neck of femur, vertebrae of the lumbar spine, and occasionally the wrist.
Low traumatic fractures are a significant risk worldwide, with 1 in 4 women and 1 in 5 men over 50 years old expected to sustain a fracture at some point in their lives. The impact of a fracture on an individual can result in fear avoidance of certain activities, loss of confidence, reduced mobility, strength, and functional capacity, a reduced quality of life, and depression or anxiety.
Exercise is one of the most effective non-pharmacological lifestyle changes that can influence bone strength and reduce the risk of fracture and falls, increase functional strength, improve confidence, reduce anxiety and depression, and improve overall quality of life. The Australian guidelines for physical activity recommend a minimum of 150 minutes per week of moderate-intensity aerobic exercise and at least two resistance training sessions per week to maintain a healthy life. However, exercise recommendations for osteoporosis focus on progressive resistance training, progressive impact training, and balance type activities.

To optimize your bone health exercise plan, seek out an Accredited Exercise Physiologist or Physiotherapist who specializes in exercise for osteoporosis.
At Nordica Health we complete a health screen and a thorough assessment will help tailor the exercise plan to your individual needs and preferences. Your starting point and maintenance phase will depend on your risk factors and individuality.
Taking action to improve your bone health can reduce the risk of low traumatic fracture and improve your overall quality of life.
0 0 votes Article Rating
What is National Pain Week? In support of National Pain Week, on the 27th of July, the staff at Nordica Health will come together to…
Osteoporosis Osteoporosis, often referred to as a “silent disease,” is a condition that quietly weakens bones, making them susceptible to low-trauma fractures. These fractures can…
Our exercise physiologists on the Sunshine Coast provide health screening and testing, and together you will create your health plan that suit your needs and preferences.
Mon-Fri 6:30 am – 6:00 pm
Please bear in mind that we may be busy with clients and we do our best to attend to your phone call. Please leave a message and we will get back to you.