Characteristics of Osteoporosis
Osteoporosis is a disease characterised by low bone mass and structural deterioration of bone tissue, leading to increased fragility and susceptibility to fractures. It is estimated that over 200 million people worldwide are living with osteoporosis. Proper diagnosis of osteoporosis is crucial for timely intervention and management of the condition.
Bone Mineral Density (BMD) in osteoporosis
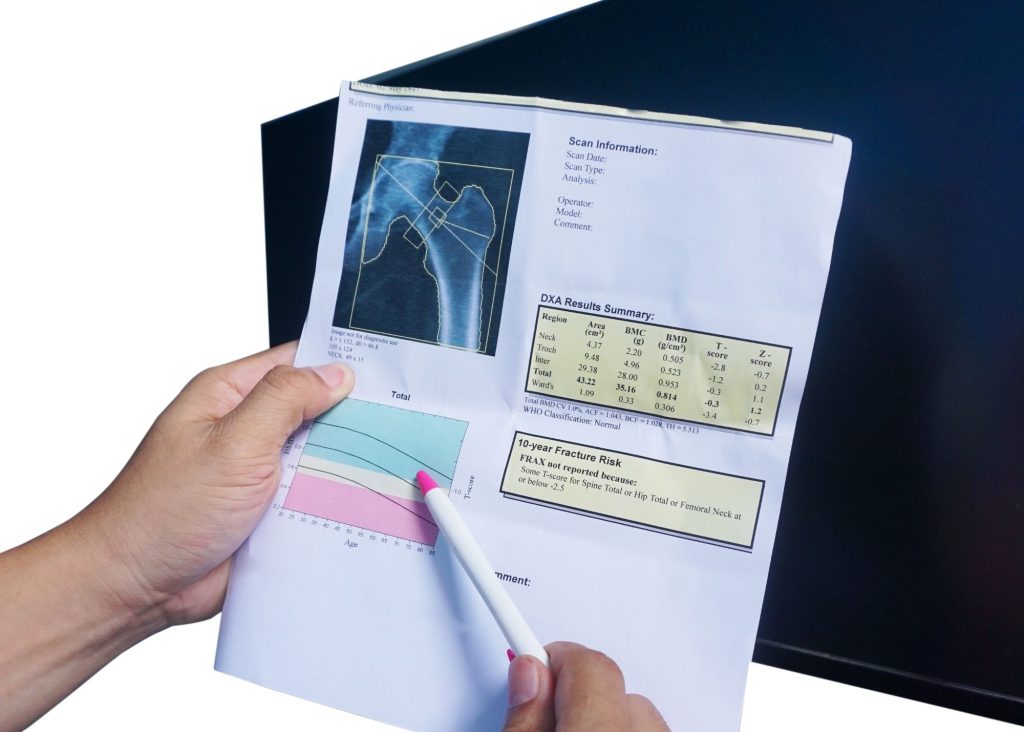
Bone Mineral Density (BMD) testing is the gold standard for diagnosing osteoporosis. BMD is one determinant of bone strength. This test measures the density of minerals, such as calcium, in the bones. Dual-energy X-ray absorptiometry (DXA) scans are commonly used to assess BMD at the hip, lumbar spine, and wrist. The World Health Organization (WHO) defines osteoporosis as a BMD of 2.5 standard deviations below the mean, typically indicated by a T-score of -2.5 or lower. A T-score between -1.0 and -2.5 indicates osteopenia, a precursor to osteoporosis. While DXA scans are readily available and non-invasive with low radiation exposure, they only provide a two-dimensional measurement of BMD at specific sites, which may not fully represent overall bone health when used alon
The natural curve of bone mineral density from childhood to adulthood
The natural curve of bone mineral density follows a pattern from childhood to adulthood. During childhood and adolescence, the body typically produces more osteoblasts (cells responsible for bone formation) than osteoclasts (cells responsible for bone breakdown), resulting in a net gain of bone mass and density. However, as we approach our late 20s or early 30s, the rate of bone formation slows down, and the balance shifts towards osteoclasts. This leads to a plateau and possible decline in bone mineral density. There are several factors that will play a role in how quickly our net BMD will decline, which can possibly result in a reduced bone strength and increased risk of fracture.
Low traumatic fractures in osteoporosis
While BMD testing is valuable, it has limitations when used in isolation to predict fracture risk accurately. To address this, the National Bone Health Alliance has proposed expanding the diagnostic criteria for osteoporosis. They suggest considering low-trauma fractures as diagnostic indicators, even without meeting the traditional BMD criteria. For instance, a low-trauma hip fracture, with or without a BMD test, is considered diagnostic of osteoporosis. The presence of low-trauma clinical vertebral fractures, proximal humerus fractures, or pelvis fractures in individuals with osteopenia may also indicate osteoporosis. Additionally, a low-trauma distal forearm fracture in a person with osteopenia at the lumbar spine or hip may be considered diagnostic in certain cases.
Low-trauma fractures, also known as fragility fractures, occur due to minimal force or trauma, such as a fall from standing height or minor impact. These fractures typically occur in individuals with reduced bone strength or underlying conditions like osteoporosis. Common sites for these fractures include the hip, spine, wrist, proximal humerus, and pelvis.
In addition to low-trauma fractures, healthcare professionals can utilise the Fracture Risk Assessment Tool (FRAX) to estimate an individual’s 10-year probability of experiencing major osteoporotic fractures or hip fractures.

Osteoporosis: Fracture Risk Assessment Tool (FRAX)
FRAX incorporates various clinical risk factors, including age, sex, BMI, previous fracture history, parental hip fracture, smoking status, alcohol intake, glucocorticoid use, and the presence of secondary causes of osteoporosis. It also integrates BMD measurements, when available, to provide a more accurate assessment. If an individual’s calculated 10-year probability of hip fracture is equal to or exceeds 3% or the 10-year probability of major osteoporotic fracture is equal to or exceeds 20%, it can support a diagnosis of osteoporosis, even without meeting the traditional BMD T-score criteria.
By expanding the diagnostic criteria to include low-trauma fractures and utilising tools like FRAX, a greater number of individuals at elevated fracture risk can be identified. However, it’s important to acknowledge that FRAX has limitations as well. It does not consider certain risk factors such as physical activity, falls, or muscle strength. Moreover, FRAX has primarily been developed for postmenopausal women and men over 50 years old, limiting its applicability to other populations.
Testing and Assessment to Diagnose Osteoporosis
Diagnosing osteoporosis involves a combination of diagnostic methods, including BMD testing, assessment of low-trauma fractures, and the use of tools like FRAX. While BMD testing remains the gold standard, the inclusion of low-trauma fractures and fracture risk assessment tools helps improve the accuracy of diagnosing osteoporosis and identifying individuals at high risk of fractures.
Sunshine Coast Clinic Specialising in Osteoporosis
Nordica Health Clinic is an Exercise Physiology clinic on the Sunshine Coast, specialising in helping individuals with Osteoporosis live a quality life with minimal pain. Our Exercise Physiologists use evidence based testing and practices to together with their clients develop an individualised training program, individually and in groups.
Contact Nordica Health Clinic in Forest Glen, Sunshine Coast, to find out more how we can assist you on your osteoporosis journey.
Get in Touch

Location
Clinic Address : Forest Glen Village Centre Tenancy B2, 354 Mons Road Forest Glen, Sunshine Coast, QLD 4556

Phone / Fax
Phone: 0477 783 799
Fax: 07 5335 1675
admin@nordicahealth.com.au





