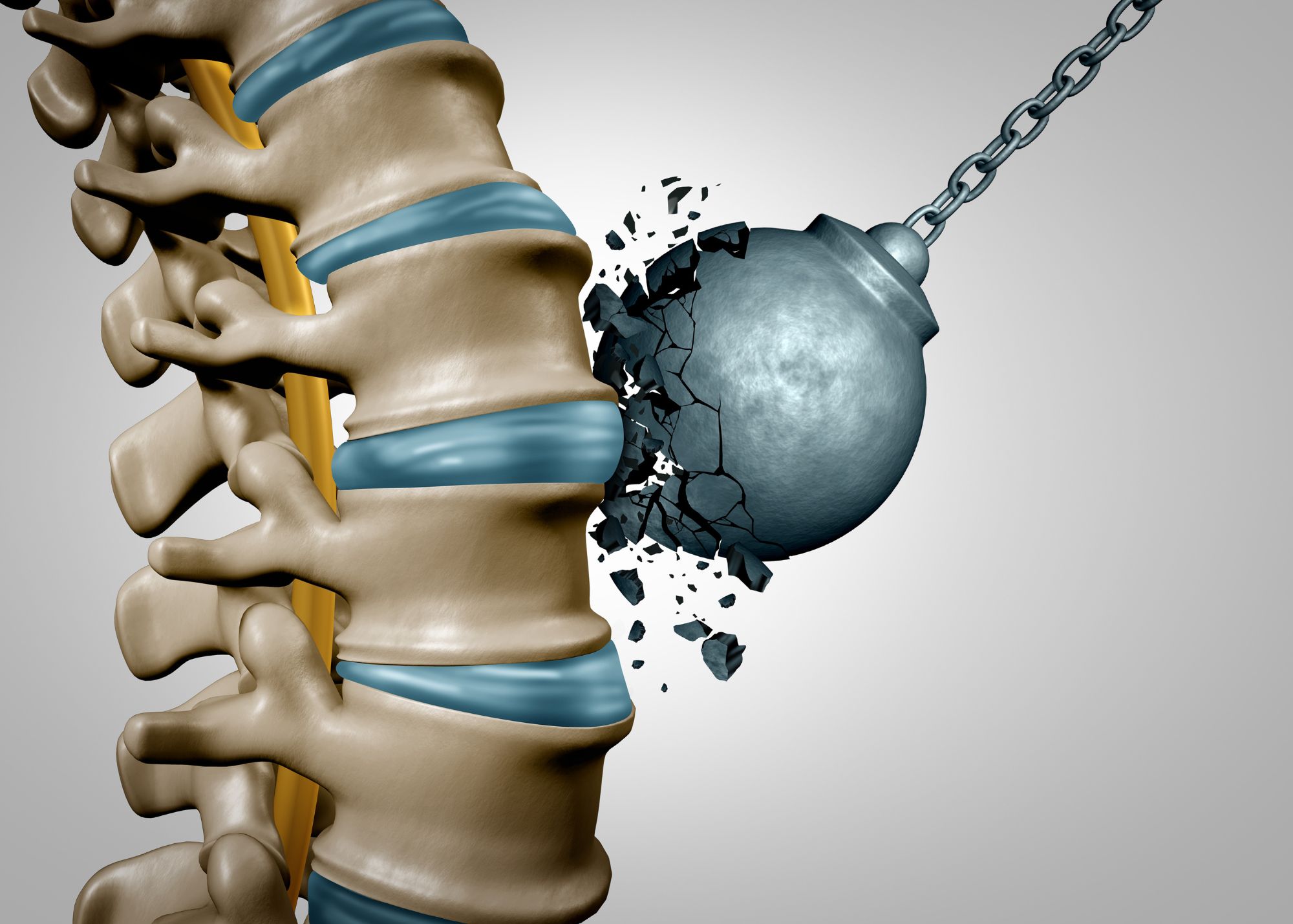
Bone strength is essential for maintaining a healthy skeletal system and plays a crucial role in supporting our body’s structure, protecting vital organs, and facilitating movement. While bones may appear solid and unyielding, they possess dynamic properties that contribute to their overall strength and integrity.
In this post, we will delve into four significant factors that contribute to bone strength: bone mineral density (BMD), bone microarchitecture, bone turnover, and bone quality. Each of these characteristics plays a distinct role in determining the overall strength and resilience of our bones.
Bone Mineral Density (BMD)
Bone Mineral Density (BMD) is a measure of the amount of minerals (such as calcium) in bone tissue. Higher BMD generally indicates stronger bones. BMD is most commonly measured through a dual-energy X-ray absorptiometry (DXA) scanner at the hip, the lumbar spine, and occasionally the wrist. DXA is accessible, easy to use, and a relatively non-invasive procedure with low radiation exposure. It’s useful for monitoring changes in bone health and assessing fracture risk over time. However, DXA limitations include measuring only two-dimensional BMD at the hip and spine, which may not represent overall bone health accurately. Also, it may not detect changes in bone microarchitecture or quality, which can affect bone strength and fracture risk.
Bone microarchitecture
Bone microarchitecture refers to the microscopic structure of bone tissue, including the organisation and arrangement of bone cells and the mineralised bone matrix. Good bone microarchitecture typically involves well-organised, dense trabecular (spongy) bone and thick, strong cortical bone. TBS (Trabecular Bone Score) and HR-pQCT (High-Resolution Peripheral Quantitative Computed Tomography) are two different methods for assessing bone microarchitecture. TBS is a software-based technique that uses standard DXA images to provide information on trabecular bone microarchitecture, while HR-pQCT is a specialised imaging technique that creates high-resolution 3D images of both trabecular and cortical bone microarchitecture. TBS is relatively low-cost and non-invasive, while HR-pQCT provides more detailed information on bone microarchitecture.
Bone turnover
Bone turnover refers to the natural process of bone remodeling, which involves a balance between bone formation and bone resorption, regulated by our bone cells. When this balance is disrupted, such as in the case of excessive bone resorption, bone strength may be compromised. Bone turnover can be assessed by measuring markers of bone formation and resorption. These markers can be measured using blood and urine tests, and they provide information on the rate of bone turnover. Examples of bone formation markers include osteocalcin, P1NP, and BSAP, while examples of bone resorption markers include CTX, NTX, and DPD. However, it’s important to note that these markers can be influenced by various factors such as age, sex, menopausal status, certain medications, and medical conditions.
Bone quality
Bone quality is a broad term that encompasses several factors, including the composition and organisation of bone tissue, the number and organisation of bone cells, and the overall health and function of bone tissue. Bone quality can be assessed using a variety of methods, including bone biopsy, imaging techniques, and biochemical markers. Imaging techniques such as DXA, HR-pQCT, and TBS can provide indirect measures of bone quality by assessing bone density, microarchitecture, and texture, respectively. Biochemical markers, such as advanced glycation end products (AGEs), can provide information on the quality of the bone matrix. Other factors that can impact bone quality include the composition and organisation of the bone tissue, the presence of microdamage or other defects, and the presence of comorbidities that can affect bone health, such as kidney disease or diabetes.

Bone mineral density (BMD) serves as a fundamental measure of bone health, reflecting the mineral content within bone tissue. However, while BMD measurements through DXA scanning provide accessible and non-invasive assessments, they may not capture the full complexity of bone health, such as changes in microarchitecture and quality. A balance between bone formation and resorption is important for maintaining healthy bone turnover, while bone quality depends on several factors related to bone tissue composition and organisation. Higher bone mineral density and well-organised, dense trabecular and cortical bone are all factors influencing bone strength.